What is Mpox [MonkeyPox] ?
As a viral zoonotic illness, monkeypox is spread from animals to people. The orthopoxvirus family, which also includes the smallpox virus, is the source of the monkeypox virus. The disease was initially discovered in 1958 in lab monkeys, which is how it acquired its name. Monkeys are only unintentional hosts; rodents and other small mammals are thought to be its main carriers. 1970 saw the identification of the first human case in the Democratic Republic of the Congo (DRC).
We will examine several facets of monkeypox in this thorough review, including its causes, spread, symptoms, management, avoidance, and current significance for public health.
Origins of Monkeypox :
It is indigenous to Central and West Africa, where people are more likely to come into touch with sick animals in regions with lush tropical rainforests. Human infections are rather uncommon; animals are the primary hosts of the virus. Monkeypox initially struck humans in the Democratic Republic of the Congo (DRC) in 1970. Since then, outbreaks have occasionally been documented in other African nations, especially in rural areas where people frequently come into touch with wild animals.
Monkeypox cases in humans had been uncommon outside of Africa until more recent breakouts around 2022. Previously, sporadic occurrences had been connected to the exotic pet trade or tourists from endemic areas. For instance, the importation of diseased animals, mostly prairie dogs, resulted in an outbreak of monkeypox in the United States in 2003.
Also Read : How AI [Artificial intelligence] Changing Our Life ? Complete Information
Transmission of Monkeypox :
There are different ways that monkeypox can spread, depending on the situation, from humans to animals or from person to person.
1. Animal-to-Human Transmission: Direct contact with an infected animal’s blood, body fluids, or skin lesions can result in the transmission of monkeypox to humans. This may occur when handling diseased pets or wildlife, hunting, or preparing bushmeat. Primates, especially monkeys, can also contract the virus, but rats, squirrels, and dormice are thought to be the primary reservoirs.
2. Human-to-Human Transmission: Although less infectious than smallpox, monkeypox can nevertheless spread from person to person. Since its primary mode of transmission is large respiratory droplets, which are limited to a few feet in length, prolonged face-to-face contact is typically required. Direct contact with bodily fluids, sores, or contaminated objects like clothing or bedding can also spread the infection. Sexual contact has been the means of transmission in certain occasions, particularly in intimate situations.
3.Vertical Transmission: The virus can also pass from a pregnant mother to her fetus via the placenta, which may lead to congenital monkeypox.
Monkeypox is not as highly transmissible as other viruses like measles or COVID-19, but outbreaks can still occur, especially in populations with lower immunity to orthopoxviruses, such as those born after the eradication of smallpox.
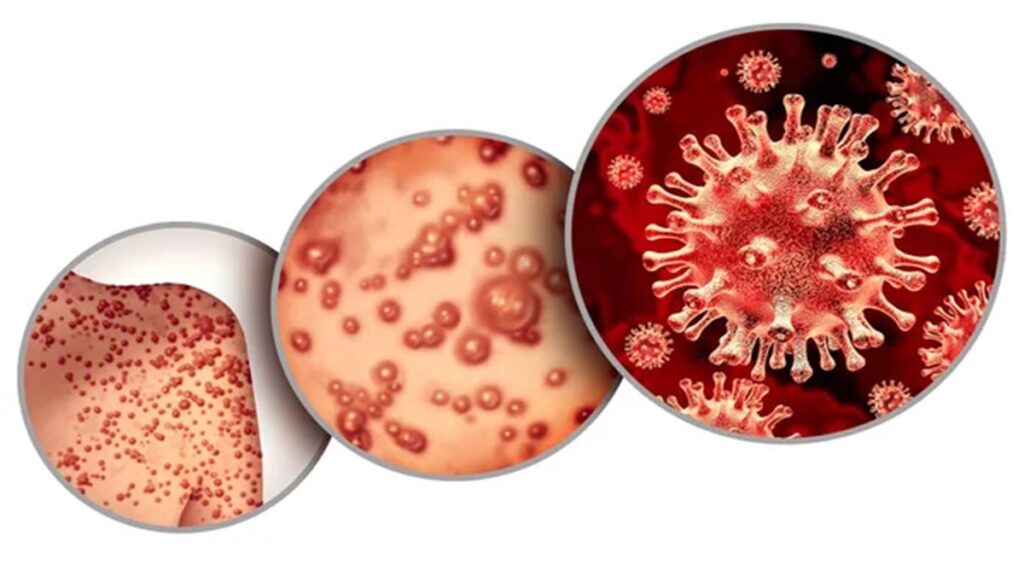
Symptoms of Monkeypox :
The incubation period of monkeypox typically ranges from 5 to 21 days, with an average of 6 to 13 days. The disease progresses through two phases: the invasion phase and the skin eruption phase.
- Invasion Phase: This stage lasts for 1 to 5 days and is characterized by non-specific symptoms such as:
- FeverHeadacheMuscle aches (myalgia)Back painSwollen lymph nodes (lymphadenopathy) — this is a distinctive feature that differentiates monkeypox from smallpoxExhaustion
- Skin Eruption Phase: A few days after the fever begins, a rash develops, usually starting on the face and spreading to other parts of the body, including the palms of the hands and soles of the feet. The rash goes through several stages before healing:
- Macules (flat, discolored areas)
- Papules (raised bumps)
- Vesicles (fluid-filled blisters)
- Pustules (pus-filled blisters)
- Scabs that eventually fall off
In most cases, monkeypox is a self-limiting disease, with symptoms lasting between 2 and 4 weeks. However, in some cases, particularly in children, pregnant women, or individuals with weakened immune systems, the disease can become severe or even fatal.
Also Read : ChatGPT Complete Course: Mastering AI- OpenAI
Diagnosis :
A combination of clinical signs, especially the recognizable rash, and laboratory tests can be used to identify monkeypox. To distinguish monkeypox from other rash-causing illnesses like chickenpox or smallpox, laboratory confirmation is necessary. Polymerase chain reaction (PCR) testing of skin lesion or scab material is the most dependable method.
Serological tests can identify orthopoxvirus antibodies in endemic locations, but they are unable to distinguish between orthopoxviruses other than monkeypox, such smallpox or vaccinia.
Treatment and Management :
Monkeypox has no particular treatment; supportive care is the mainstay of treatment. This involves treating any secondary bacterial infections that may develop, avoiding dehydration, and controlling symptoms like pain and fever. While their efficacy against monkeypox is still being assessed, antiviral drugs created for smallpox, including tecovirimat, may be employed in specific situations.
Intravenous immunoglobulin (IVIG) and antivirals like cidofovir or brincidofovir may be tried for severe instances, especially in immunocompromised patients. However, these treatments are not commonly available.
Also Read : How to Quit Smoking – 100% Success Guarantee – Step by Step
Prevention and Vaccination :
A variety of steps are taken to minimize both human-to-human and animal-to-human transmission in order to prevent monkeypox.
Preventing Animal Transmission: It is crucial to keep humans away from wild animals, especially rats and monkeys, in regions where monkeypox is endemic. Additionally, eating bushmeat from animals that may be infected is advised. It’s important to cook meat correctly and follow food safety procedures.
Human-to-Human Transmission: To stop the spread of monkeypox in outbreak situations, infected persons should be isolated, healthcare personnel should wear personal protective equipment (PPE), and excellent cleanliness practices are crucial. Bedding and clothes that have been contaminated should be handled carefully and cleaned properly.
Vaccination: Due to the close relationship between the two viruses, the smallpox vaccination historically offered cross-protection against monkeypox. As a result of mass vaccination campaigns ending in 1980 when smallpox was eradicated, the world’s population’s immunity to orthopoxviruses declined. Nonetheless, more recent vaccinations have been created and are authorized for use against smallpox and monkeypox, such as the modified vaccinia Ankara (MVA) vaccine. As a preventive strategy, these vaccines may be made available to high-risk individuals, such as laboratory personnel handling orthopoxviruses and healthcare workers.
Following the 2022 outbreaks, some nations have also begun to provide the monkeypox vaccine to those who are more vulnerable, such as men who engage in male-to-male sex (MSM) and those who have already been exposed to the virus.
Public Health Impact :
The pandemic of monkeypox has become a major public health concern, especially after instances were detected in several non-endemic nations in 2022. Health officials were alarmed by this worldwide spread since it indicated that the virus was spreading across human populations more readily than previously believed.
The causes of this change are still being investigated, however some elements are as follows:
decreased resistance to orthopoxviruses when smallpox immunization campaigns were discontinued.
The spread of zoonotic illnesses may be aided by modifications in human behavior and environmental elements such greater interaction with wildlife, urbanization, and deforestation.
Possible alterations to the virus itself, despite the fact that no obvious mutations have been found that would explain the rise in transmission.
Global Response :
The World Health Organization (WHO) declared monkeypox a public health emergency of international concern (PHEIC) in response to the coordinated worldwide response to the outbreaks in 2022. Containment has been the main goal of public health initiatives, which have included contact tracing, immunization, case isolation, and public awareness campaigns to inform the public about the dangers of transmission.
Working together internationally, governments, researchers, and health organizations has been crucial to comprehending the changing epidemiology of monkeypox and putting containment plans into action. Research on the virus, vaccines, and treatment alternatives has increased, and surveillance systems have been reinforced.
Conclusion :
Once an uncommon zoonotic disease, monkeypox has drawn interest from all around the world as a result of its increased transmission and the 2022 epidemic in non-endemic areas. Monkeypox is often less severe and contagious than smallpox, despite many similarities between the two illnesses. But since smallpox vaccination programs have ended, people’s immunity against orthopoxviruses has decreased, making the virus a greater hazard to public health.
The primary methods of controlling monkeypox include vaccination, case isolation, and public health education. These strategies aim to prevent transmission from animals to humans as well as humans to humans. In order to control future outbreaks, further research on efficient therapies and vaccinations will be essential. Understanding the ecology of the virus, along with strengthening global health systems to respond to emerging infectious diseases, is key to preventing monkeypox from becoming a larger and more persistent public health challenge.